It’s all in your head. That’s what you’re told when what you think is perceived not to matter. Funny how prescient those beliefs become: sometimes what you think is the only thing that matters.
Take the buzz around the CDC opioid prescribing guidelines. They’re a veritable Rorschach test. For some, they’re too lenient. For others, they’re too strict. But mostly they’re a reflection of what people think about opioids for the treatment of acute and chronic pain.
Over the recent weeks, we surveyed readers to glean their thoughts on their care experience when it comes to all things pain related. We asked a series of questions, roughly one per week, with the intent of ascertaining what people thought about their pain management.
The results were predictably unpredictable. Nearly every result contained some degree of selection bias. This is almost impossible to avoid when conducting open sourced online surveys. But we found something more valuable hidden just beneath the numbers themselves, within the bias. By looking at the range of responses rather than the responses themselves, we found an interesting trend in the asymmetry that appeared.
It’s something statisticians call skewness and it’s one of those terms we learn and then quickly forget. But when we analyze the responses by the curves they produce once graphed out, we find important trends in the underlying perception of the respondents. These trends explain why we repeatedly see a disparity between the care patients receive and their perceptions of their pain treatment. Let’s start by comparing the relative frequency of the most common response to each question.
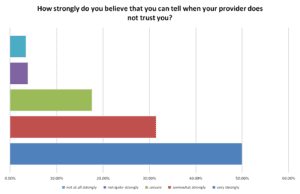
At first blush, the response to the question, “How strongly do you believe that you can tell when your provider does not trust you?”, may prompt a certain level of obvious indifference. However, the most frequent response, ‘very strongly’, came in at 49.33 percent, just under half.
Compare that with the most frequent responses for the following three questions:
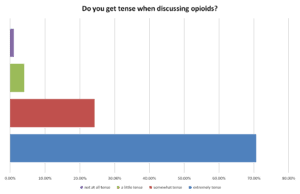
- Do you get tense when discussing opioids?
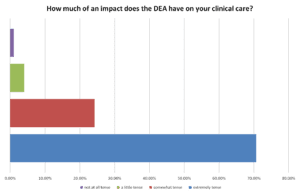
- How much of an impact does the DEA have on your clinical care?
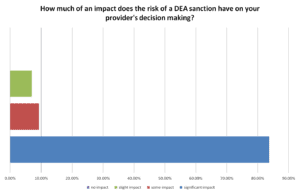
- How much of an impact does the risk of a DEA sanction have on your provider’s decision making?
For these three questions, the most extreme response was also the most frequent, but it was much more frequent than the first question: 70.71 percent, 82.56 percent, and 83.72 percent, respectively, to be exact. The responses indicate a clear bias in the survey design. But the point isn’t that the responses are skewed. Instead, focus on the degree of skewness, which varies for each of these four questions. These variances reveal which perceptions dominate over others.
Note how respondents believe the influence of the DEA has a greater impact on their care than the mutual trust between a provider and a patient. The disparity is over 10 percent, not an insignificant amount. Clearly, the DEA plays a significant role in influencing the patient-physician encounter.
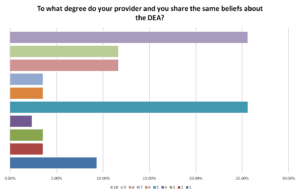
Now look at the question where we asked the degree to which providers and patients share similar beliefs about the DEA. Again, we see a skewing toward the extremes, revealing an inherent survey bias. But the gradual increase toward the upper extreme, 10, shows a clear trend toward sharing similar views: that both the provider and patient share similar views about the DEA.
1
9.30%
2
3.49%
3
3.49%
4
2.33%
5
25.58%
6
3.49%
7
3.49%
8
11.63%
9
11.63%
10
25.58%
Each of the response patterns, when viewed only in reference to the question asked, appears obvious. But when the response patterns are viewed side by side, they expose certain contradictions – that may actually make sense, but only if you consider the adverse effects the DEA has on clinical care.
One question asks whether patients feel tense when discussing opioids with their providers, and skews strongly toward ‘tense’ and ‘very tense’. Another question asks about the degree to which a provider and a patient share similar beliefs about the DEA, which found a strong trend toward the two sharing similar beliefs.
But why would patients feel tense when discussing opioids if the majority of the respondents share similar views as their providers about them?
The contradictory answers expose a certain disingenuousness that appears in patient encounters for nearly all chronic pain patients. Patients and providers both know of the stigmatization chronic pain patients experience. They see it, they acknowledge it, yet they do nothing about it. They taper opioid prescriptions when they know it causes patient harm. They lower doses without any clinical rationale to do so.
Both providers and patients are acutely aware that providers make prescribing decisions to avoid legal liability rather than to do what’s best for the patient clinically. Yet few will admit as much. It’s a shame that it takes a survey to say what most in the medical community will not. Their silence is as extreme as the skews in the distribution curves.
True, these surveys are far from the traditional Likert surveys commonly seen in peer reviewed academic studies. These surveys contain dirty data, as many behavioral economists would label it: responses laced with biases and filled with subjective perceptions unique to each individual. It’s not truly objective. It’s not supposed to be. Yet, it’s a highly accurate gauge of the patient experience.
Sometimes the biases in our heads are the only things that matter. So the next time someone says – it’s all in your head – tell them they’re right, and tell them that’s why it matters.
Full Data – Gathered between September 2022 and December 2022
How strongly do you believe that you can tell when your provider does not trust you?
49.93% very strongly
31.38% somewhat strongly
17.57% unsure
3.77% not quite strongly
3.35% not at all strongly
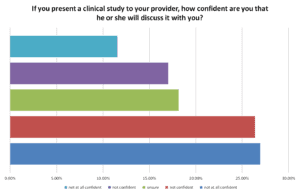
If you present a clinical study to your provider, how confident are you that he or she will discuss it with you?
26.92% not at all confident
26.37% not confident
18.13% unsure
17.03% somewhat confident
11.54% very confident
Do you get tense when discussing opioids?
70.71% extremely tense
24.24% somewhat tense
4.04% a little tense
1.01% not at all tense
How much of an impact does the DEA have on your clinical care?
82.56% significant impact
11.63% some impact
4.65% slight impact
1.16% no impact
How much of an impact does the risk of a DEA sanction have on your provider’s decision making?
83.72% significant impact
9.30% some impact
6.98% slight impact
0% no impact
To what degree do your provider and you share the same beliefs about the DEA?
1
9.30%
2
3.49%
3
3.49%
4
2.33%
5
25.58%
6
3.49%
7
3.49%
8
11.63%
9
11.63%
10
25.58%
















The patient has no rights. The Dr is prepared. When he wants to take ones pain medication away he steers the conversation so any reasoning the sufferer attempts makes him appear as a pleading addict. It’s a one-sided psychological game where the Dr always gets his way. Patient walks into appointment filled with hope of getting relief and leaves feeling like a (guilty) victim, now suffering even more because he has less medication than when he made the appointment. Sad! The patients empathize, they don’t want to see the Dr lose a career he has dedicated so many years of his life to. Sad! Dr’s aren’t honoring the oath they took-it’s akin to having a knife at their throats. So sad!! Think about it, both Dr and patient have their quality of life taken away. Suicides are on the rise on both sides.