As abortion bans go into effect across a contiguous swath of the South, cancer physicians are wrestling with how new state laws will influence their discussions with pregnant patients about what treatment options they can offer.
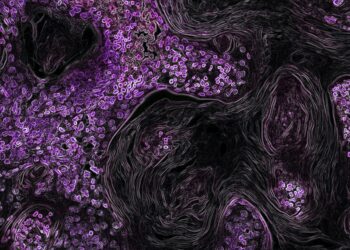
Cancer coincides with roughly 1 in 1,000 pregnancies, most frequently breast cancer, melanoma, cervical cancer, lymphomas, and leukemias. But medications and other treatments can be toxic to the developing fetus or cause birth defects. In some cases, hormones that are supercharged during pregnancy fuel the cancer’s growth, putting the patient at greater risk.
Although new abortion restrictions often allow exceptions based on “medical emergency” or a “life-threatening physical condition,” cancer physicians describe the legal terms as unclear. They fear misinterpreting the laws and being left in the lurch.
For instance, brain cancer patients have traditionally been offered the option of abortion if a pregnancy might limit or delay surgery, radiation, or other treatment, said Dr. Edjah Nduom, a brain cancer surgeon at Emory University’s Winship Cancer Institute in Atlanta.
“Is that a medical emergency that necessitates the abortion? I don’t know,” Nduom asked, trying to parse the medical emergency exception in the new Georgia law. “Then you end up in a situation where you have an overzealous prosecutor who is saying, ‘Hey, this patient had a medical abortion; why did you need to do that?’” he said.
Pregnant patients with cancer should be treated similarly to non-pregnant patients when feasible, though sometimes adjustments are made in the timing of surgery and other care, according to a research overview, published in 2020 in Current Oncology Reports.
With breast cancer patients, surgery could be performed early on as part of the treatment, pushing chemotherapy to later in the pregnancy, according to the research. Cancer experts typically recommend avoiding radiation therapy throughout pregnancy, and most chemotherapy drugs during the first trimester.
But with some cancers, such as acute leukemia, the recommended drugs have known toxic risks to the fetus, and time is not on the patient’s side, said Dr. Gwen Nichols, chief medical officer of the Leukemia & Lymphoma Society.
“You need treatment urgently,” she said. “You can’t wait three months or six months to complete a pregnancy.”
Another life-threatening scenario involves a patient early in her pregnancy who has been diagnosed with breast cancer that’s spreading, and tests show that the cancer’s growth is spurred by the hormone estrogen, said Dr. Debra Patt, an oncologist in Austin, Texas, who estimated she has cared for more than two dozen pregnant patients with breast cancer.
“Pregnancy is a state where you have increased levels of estrogen. It’s actually actively at every moment causing the cancer to grow more. So I would consider that an emergency,” said Patt, who is also executive vice president over policy and strategic initiatives at Texas Oncology, a statewide practice with more than 500 physicians.
When cancer strikes individuals of child-bearing age, one challenge is that malignancies tend to be more aggressive, said Dr. Miriam Atkins, an oncologist in Augusta, Georgia. Another is that it’s unknown whether some of the newer cancer drugs will affect the fetus, she said.
While hospital ethics committees might be consulted about a particular treatment dilemma, it’s the facility’s legal interpretation of a state’s abortion law that will likely prevail, said Micah Hester, an expert on ethics committees who chairs the department of medical humanities and bioethics at the University of Arkansas for Medical Sciences College of Medicine in Little Rock.
“Let’s be honest,” he said. “The legal landscape sets pretty strong parameters in many states on what you can and cannot do.”
It’s difficult to fully assess how physicians plan to handle such dilemmas and discussions in states with near-total abortion bans. Several large medical centers contacted for this article said their physicians were not interested or not available to speak on the subject.
Other physicians, including Nduom and Atkins, said the new laws won’t alter their discussions with patients about the best treatment approach, the potential impact of pregnancy, or whether abortion is an option.
“I’m going to always be honest with patients,” Atkins said. “Oncology drugs are dangerous. There are some drugs that you can give to [pregnant] cancer patients; there are many that you cannot.”
The bottom line, maintain some, is that termination remains a critical and legal part of care when cancer threatens someone’s life.
Patients “are counseled on the best treatment options for them, and the potential impacts on their pregnancies and future fertility,” Dr. Joseph Biggio Jr., chair of maternal-fetal medicine at Ochsner Health System in New Orleans, wrote in an email. “Under state laws, pregnancy termination to save the life of the mother is legal.”
Similarly, Patt said that physicians in Texas can counsel pregnant patients with cancer about the procedure if, for instance, treatments carry documented risks of birth defects. Thus, physicians can’t recommend them, and abortion can be offered, she said.
“I don’t think it’s controversial in any way,” Patt said. “Cancer left unabated can pose serious risks to life.”
Patt has been educating physicians at Texas Oncology on the new state law, as well as sharing a JAMA Internal Medicine editorial that provides details about abortion care resources. “I feel pretty strongly about this, that knowledge is power,” she said.
Still, the Texas law’s vague terminology complicates physicians’ ability to determine what’s legally permissible care, said Joanna Grossman, a professor at SMU Dedman School of Law. She said nothing in the statute tells a doctor “how much risk there needs to be before we label this legally ‘life-threatening.’”
And if a woman can’t obtain an abortion through legal means, she has “grim options,” according to Hester, the medical ethicist. She’ll have to sort through questions like: “Is it best for her to get the cancer treatment on the time scale recommended by medicine,” he said, “or to delay that cancer treatment in order to maximize the health benefits to the fetus?”
Getting an abortion outside Georgia might not be possible for patients with limited cash or no backup child care or who share one car with an extended family, Atkins said. “I have many patients who can barely travel to get their chemotherapy.”
Dr. Charles Brown, a maternal-fetal medicine physician in Austin who retired this year, said he can speak more freely than practicing colleagues. The scenarios and related unanswered questions are almost too numerous to count, said Brown, who has cared for pregnant women with cancer.
Take as another example, he said, a potential situation in a state that incorporates “fetal personhood” in its law, such as Georgia. What if a patient with cancer can’t get an abortion, Brown asked, and the treatment has known toxic effects?
“What if she says, ‘Well, I don’t want to delay my treatment — give me the medicine anyway,’” Brown said. “And we know that medicine can harm the fetus. Am I now liable for harm to the fetus because it’s a person?”
Whenever possible, physicians have always strived to treat the patient’s cancer and preserve the pregnancy, Brown said. When those goals conflict, he said, “these are gut-wrenching trade-offs that these pregnant women have to make.” If termination is off the table, “you’ve removed one of the options to manage her disease.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Subscribe to KHN’s free Morning Briefing.