In healthcare, the distribution of burdens should account for actual risks and perceived risks that may occur when implementing a law into clinical practice. Balancing the clinical burdens with the clinical risks, both actual risk, that is obvious and apparent, and perceived risk, which is often a secondary effect and less easily defined.
The courts have maintained a balance between complex healthcare behavior and the laws that attempt to regulate them. Often ruling against excessive encroachment, which Justice Samuel Alito called, “rule by executive fiat”, when explaining many of the COVID-19 restrictions and mandates enforced by state and federal governments. The pandemic exposed many of the problems underlying healthcare, least of all our tendency for extreme simplifications.
Mask mandates, initially a guideline recommendation intended to minimize the spread of COVID-19, became a cultural referendum on the first amendment. Soon the extreme views on masks mandates reduced an epidemiological argument into a political standoff. With one side advocating for individual rights, while the other side advocating the importance of following the science. Yet both sides have taken an essentially incomplete approaches to the issue of mask use.
Months into the pandemic, leading epidemiologists across the world finally came out in support for a balanced approach to the behavioral changes. Advocating that rather than enforcing widespread economic lockdowns of society, we should advocate for selective economic restrictions for a limited period. And rather than succumb to the tyranny of the majority or the tyranny of science, we should balance the economic and medical factors that impact society.
A balance we could not quite appreciate until we saw the effects of a unilateral, extreme approach to the pandemic. Restrictive laws inevitably change the focus of clinical behavior from the behavior itself to the undue burdens imposed by the law. Often failing to understand all the potential consequences because we fail to understand all the medical issues underlying healthcare behavior.
But simply providing more information will harm as much as it will help. Seema Verma, the former head of the Centers for Medicare and Medicaid Services, wrote an op-ed in late 2019 touting the virtues of price transparencies in healthcare, and compared patient decision-making in healthcare to purchasing a car. Though most car owners are not familiar with every detail in their cars, they are familiar enough to be able to make purchasing decisions.
Healthcare decision-making is far more complex than purchasing a car, and most are far less familiar with the economics of the healthcare industry and pricing models for medical goods and services. Emphasizing price disclosures without any context or education places an intellectual burden on patients to make sense out of a complex, nuanced numbers.
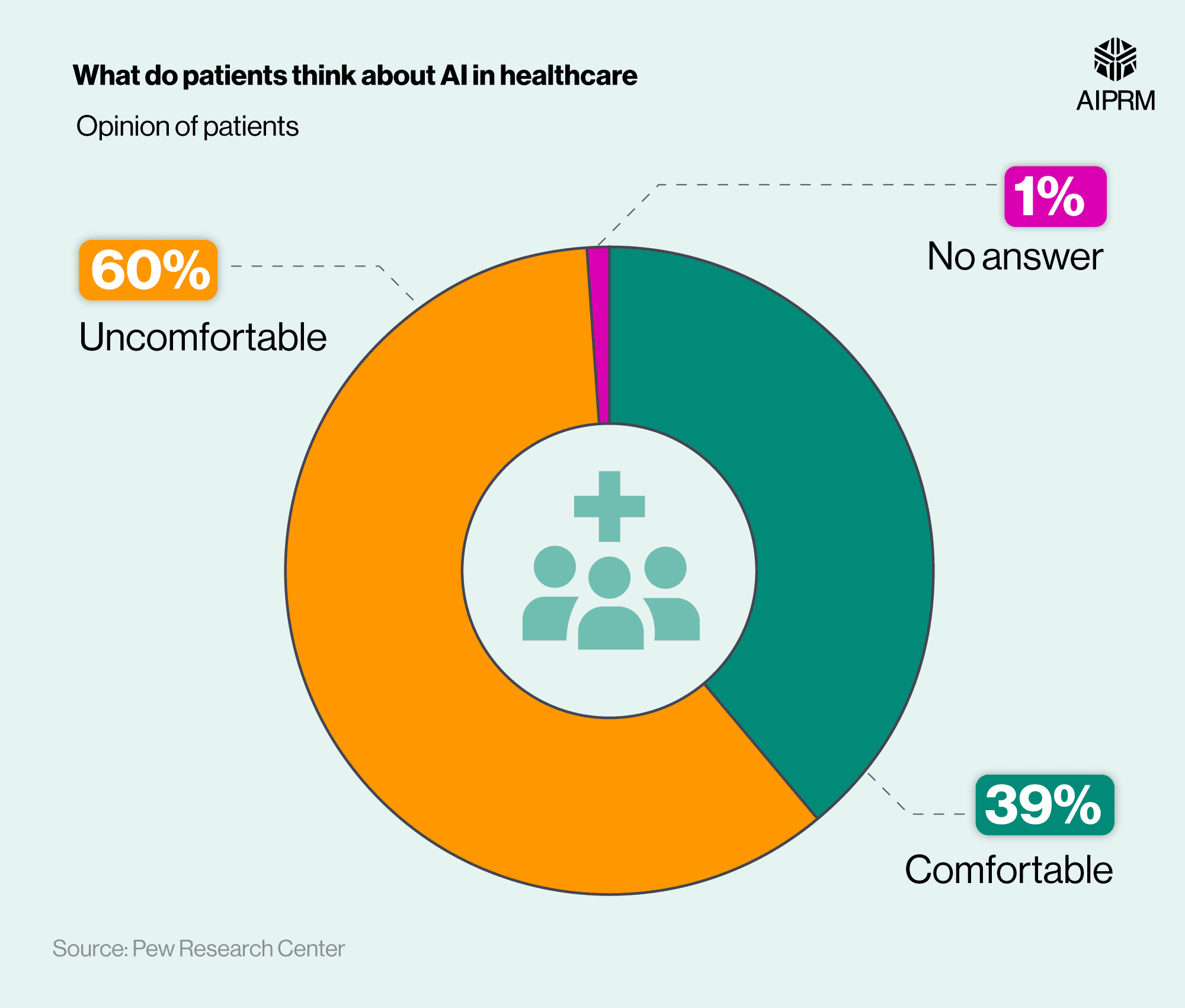
Without any basic understanding or educational training, patients will struggle to make decisions based regarding price disclosures without any support or guidance. Inevitably most patients with reference their healthcare providers or healthcare system to make sense of the numbers. In the end, the numbers may matter less than more subjective criteria such as comfort or ease with a provider or system.
For the medically indigent populations of Chicago, the hospital of choice is John Stroger Cook County, which manages a high percent of the uninsured and indigent in the city. As a nonprofit organization, Cook County hospital enjoys certain tax breaks that come from managing such patients, helping to offset any financial burdens the hospital may face.
But Cook County is not the only hospital that enjoys nonprofit status in the city, yet it is the only hospital that sees so many of the type of patients that allow hospitals to qualify as a nonprofit. When we analyze the socioeconomic status of patients admitted to hospitals across the city, we see one hospital bearing nearly all the financial burden, with the rest providing care to the absolute minimum number of uninsured and indigent patients necessary.
The purpose of price transparency is to help patients make more informed decisions regarding the cost of care. But for the most cost sensitive patients in Chicago, the indigent and uninsured, the decision has already been made. And price disclosures may be of little value.
For patients with a greater willingness to switch healthcare systems, the price disclosures may be valuable in selecting a hospital. But only valuable if they can understand the prices disclosed. If hospitals are keen to maximize profit, it is unlikely they would be as keen to share pricing data that may be averse to their bottom line. And may format the numbers to look as appealing as possible, obfuscating the original intent of pricing transparency in the first place.
The intention of pricing transparency may have been to empower patients to make more cost-effective decisions regarding their health. But in practice, the law may predispose hospitals to arrange the data to look more cost-effective. Patients not familiar with pricing models in hospitals would then bear the burden of understanding the information present, which may prove an undue burden for many patient. Who in the end may simply default to hospitals with which they were already familiar.
Complexity in healthcare creates a burden for patients that most seek to simplify or to delegate for assistance. But simplifying and delegating creates yet another burden. With each attempt to address the issue merely recontextualizing the issue. If we believe patients should have access to data to make their own decisions, then we need to explain the data. But explaining the data requires having someone to explain the data objectively. And in explaining the data objectively, we need to ensure that the patients understand the data sufficiently enough to make cost-oriented decisions. On it goes – often with the full intended consequences not manifesting until much later.
Something that played out in hospitals and courts across the country for one of the most publicized healthcare laws in recent decades, the Affordable Care Act (ACA). The law’s original keystone element, the health care insurance tax penalty, was intended to incentivize patients to get health insurance or incur a penalty. By assuming that the threat of penalty would motivate patients to purchase health insurance.
Yet even after the penalty was nullified in federal court, patients continued to purchase insurance plans through ACA insurance exchanges. And contrary to what most lawmakers believed, patient behavior improved as length of hospital stay, a metric the ACA sought to improve, reduced after the penalty was removed.
Removing the tax penalty likely had little directly impact on patient length of stay. The relationship is more likely correlative than direct cause and effect. Just like the relationship between a tax penalty and patient compliance with the ACA is more correlative than direct cause and effect.
But this tendency to simplify complex healthcare issues into laws and policies that ascribe cause and effect to complex relationships that are more correlative prevents us from understanding the full consequences of the laws and policies we enact. Consequences that prove equally impactful in the implementation as the original intention.