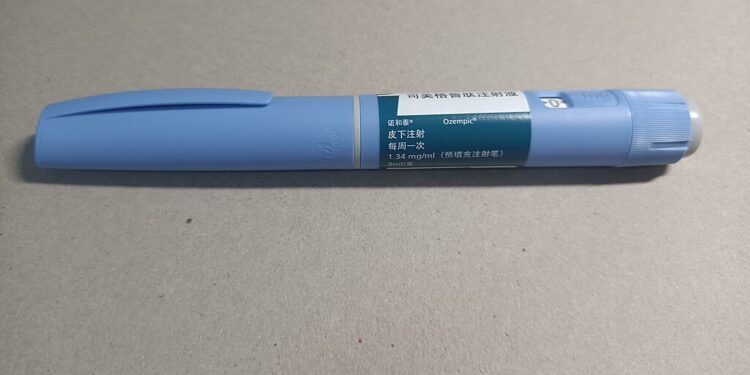
The advent of glucagon-like peptide-1 (GLP-1) receptor agonists, exemplified by medications like Ozempic (semaglutide), marks a significant milestone in the evolving landscape of peptide and hormone-based therapies in healthcare. These agents have not only transformed the management of type 2 diabetes mellitus (T2DM) and obesity but also herald a broader revolution in therapeutic strategies involving peptides and hormones. This article delves into the clinical efficacy of GLP-1 receptor agonists, explores the expanding horizon of peptide-based treatments, and examines the role of bioidentical hormones in contemporary medicine.
GLP-1 Receptor Agonists: Mechanisms and Clinical Efficacy
GLP-1 is an incretin hormone that enhances insulin secretion and suppresses glucagon release in a glucose-dependent manner, thereby regulating blood glucose levels. GLP-1 receptor agonists (GLP-1 RAs) mimic these effects, offering pharmacological levels of GLP-1 that not only improve glycemic control but also promote weight loss by delaying gastric emptying and increasing satiety. Agents such as exenatide, liraglutide, dulaglutide, and semaglutide have been developed, each administered via subcutaneous injection.
Clinical studies have demonstrated the efficacy of GLP-1 RAs in managing T2DM and obesity. For instance, a systematic review and meta-analysis by Vilsbøll et al. (2012) concluded that GLP-1 RAs effectively reduce body weight in patients with T2DM. Moreover, these agents have been associated with cardiovascular benefits, including reductions in major adverse cardiovascular events, as evidenced in trials such as the PIONEER 6 study evaluating oral semaglutide.
Beyond GLP-1: The Expanding Role of Peptide-Based Therapies
The success of GLP-1 RAs has spurred interest in other peptide-based therapies. Tirzepatide, a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, has shown promise in clinical trials, demonstrating significant weight loss and improved glycemic control in patients with T2DM. A cohort study by Zheng et al. (2023) reported that tirzepatide was associated with a lower risk of mortality and adverse cardiovascular and kidney outcomes compared to GLP-1 RAs alone.
Additionally, the development of triple agonists targeting GLP-1, GIP, and glucagon receptors, such as retatrutide, has shown unprecedented weight loss effects in phase 2 clinical trials. These advancements underscore the potential of multi-receptor targeting peptides in addressing complex metabolic disorders.
Bioidentical Hormones: Efficacy and Safety Considerations
Bioidentical hormone therapy (BHT) involves the use of hormones that are chemically identical to those produced by the human body, commonly prescribed for menopausal symptoms. While some formulations are approved by regulatory agencies, compounded bioidentical hormone therapy (cBHT) lacks such approval and is often marketed as a natural and personalized alternative.
The safety and efficacy of cBHT remain contentious. A review by the National Academies of Sciences, Engineering, and Medicine (2020) highlighted the paucity of rigorous clinical trials evaluating cBHT, emphasizing that most evidence is derived from studies on FDA-approved hormone therapies. Furthermore, concerns have been raised regarding the quality control and consistency of compounded formulations, leading to potential risks such as endometrial cancer.
Conversely, FDA-approved bioidentical hormones have been shown to be effective in managing menopausal symptoms. Clinical trials have demonstrated that estradiol, a common bioidentical hormone, effectively reduces vasomotor symptoms associated with menopause.
Challenges and Future Directions
Despite the promising developments in peptide and hormone therapies, several challenges persist. The long-term safety profiles of newer agents like tirzepatide and retatrutide require further investigation through extensive clinical trials. Additionally, the variability in patient responses necessitates personalized approaches to therapy.
In the realm of bioidentical hormones, there is a critical need for standardized formulations and rigorous clinical evaluations to ensure safety and efficacy. Healthcare providers must be vigilant in counseling patients on the potential risks associated with unregulated compounded therapies and emphasize the importance of evidence-based treatments.
Conclusion
The emergence of GLP-1 receptor agonists like Ozempic represents a pivotal advancement in peptide and hormone-based therapies, offering effective solutions for managing T2DM and obesity. The ongoing development of novel peptide agents and the utilization of bioidentical hormones further exemplify the expanding therapeutic landscape. As research progresses, it is imperative to balance innovation with rigorous evaluation to ensure that these therapies are both safe and effective for patients.
References
- Vilsbøll T, Christensen M, Junker AE, Knop FK, Gluud LL. Effects of glucagon-like peptide-1 receptor agonists on weight loss: systematic review and meta-analyses of randomised controlled trials. BMJ. 2012;344:d7771.
- Husain M, Birkenfeld AL, Donsmark M, et al. Oral Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2019;381(9):841-851.
- Zheng SL, Roddick AJ, Aghar-Jaffar R, et al. Association Between Use of Sodium-Glucose Cotransporter 2 Inhibitors, Glucagon-like Peptide 1 Agonists, and Dipeptidyl Peptidase 4 Inhibitors With All-Cause Mortality in Patients With Type 2 Diabetes: A Systematic Review and Meta-analysis. JAMA. 2018;319(15):1580-1591.