The U.S. is in the midst of a racial reckoning. The COVID-19 pandemic, which took a particularly heavy toll on Black communities, turned a harsh spotlight on long-standing health disparities that the public could no longer overlook.
Although the health disparities for Black communities have been well known to researchers for decades, the pandemic put real names and faces to these numbers. Compared with white people, Black people are at much greater risk for developing a range of health problems, including heart disease, diabetes and dementia. For example, Black people are twice as likely as white people to develop Alzheimer’s disease.
A vast and growing body of research shows that racism contributes to systems that promote health inequities. Most recently, our team has also learned that racism directly contributes to these inequities on a neurobiological level.
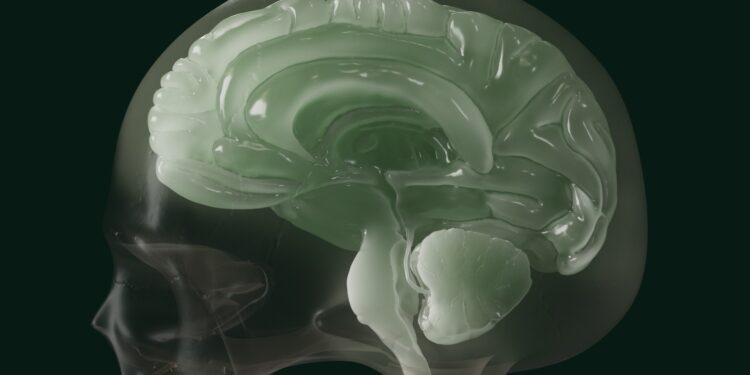
We are clinical neuroscientists who study the multifaceted ways in which racism affects how our brains develop and function. We use brain imaging to study how trauma such as sexual assault or racial discrimination can cause stress that leads to mental health disorders like depression and post-traumatic stress disorder, or PTSD.
We have studied trauma in the context of a study known as the Grady Trauma Project, which has been running for nearly 20 years. This study is largely focused on the trauma and stress of Black people in the metropolitan Atlanta, Georgia, community.
How discrimination alters the brain
Racial discrimination is commonly experienced through subtle indignities: a woman clutching her purse as a Black man walks by on the sidewalk, a shopkeeper keeping close watch on a Black woman shopping in a clothing store, a comment about a Black employee being a “diversity hire.” These slights are often referred to as microaggressions.
Decades of research has shown that the everyday burden of these race-related threats, slights and exclusions in day-to-day life translates into a real increase in disease risk. But researchers are only beginning to understand how these forms of discrimination affect a person’s biology and overall health.
Our team’s research shows that the everyday burden of racism affects the function and structure of the brain. In turn, these changes play a major role in risk for health problems.
For instance, our studies show that racial discrimination increases the activity of brain regions, such as the prefrontal cortex, that are involved in regulating emotions.

Patrick Heagney
This increased activity in prefrontal brain regions occurs because responding to these types of affronts requires high-effort coping strategies, such as suppressing emotions. People who have experienced more racial discrimination also show more activation in brain regions that enable them to inhibit and suppress anger, shock or sadness so that they can curate a socially acceptable response.
A cost for overcompensating
Despite the fact that high-energy coping allows people to manage a constant barrage of threats, this comes at a cost.
The more brain energy you use to suppress, control or manage your feelings, the more energy you take away from the rest of the body. Over time, and without prolonged periods of rest, relief and restoration, this can contribute to other problems, a process that public health researcher Arline Geronimus termed “weathering.” Having these brain regions in continual overdrive is linked with accelerated biological aging, which can create vulnerability for health problems and early death.
In our research, we have found that this weathering process is evident in the gradual degradation of brain structure, particularly in the heavily myelinated axons of the brain, known as “white matter,” which serve as the brain’s information highways.

Negar Fani
Myelin is a protective sheath around nerve fibers that allows for improved communication between brain cells. Similar to highways for vehicles, without sufficient maintenance of the myelin, degradation will occur.
Erosion in these brain pathways can affect self-regulation, making a person more vulnerable to developing unhealthy coping strategies for stress, such as emotional eating or substance use. These behaviors, in turn, can increase one’s risk for a wide variety of health problems.
These racism-related changes in the brain, and their direct effects on coping, may help to explain why Black people are twice as likely to develop brain health problems such as Alzheimer’s disease compared with white people.
Recognizing racial gaslighting
In our view, what makes racism particularly insidious and pernicious to the health of Black people is the societal invalidation that accompanies it. This makes racial trauma effectively invisible. Racism, whether it originates from people or from institutional systems, is often rationalized, excused or dismissed.
Such invalidation leads those who experience racism to second-guess themselves: “Am I just being too sensitive?” People who have the temerity to report racist events are often ridiculed or met with skepticism. This extends to academic spheres as well.
This continual questioning and doubting of the circumstances around racist experiences, or racial gaslighting, may be part of what depletes the brain of its resources, causing the weathering that ultimately increases vulnerability to brain health problems.
Interrupting this cycle requires that people learn to identify their biases toward people of color and people in marginalized groups more generally, and to understand how those biases may lead to discriminatory words and behavior. We believe that by finding their blind spots, people can see ways in which their actions and behaviors could be viewed as hurtful, exclusionary or offensive. Through recognition of these experiences as racist, people can become allies rather than skeptics.
Institutions can help to create a culture of healing, validation and support for people of color. A validating, supportive institutional culture may help people of color normalize their reactions to these stressors, in addition to the connection – and restoration – they may find within their communities.
Negar Fani, Associate Professor of Psychiatry and Neuroscience, Emory University and Nathaniel Harnett, Assistant Professor of Psychiatry, Harvard Medical School
This article is republished from The Conversation under a Creative Commons license. Read the original article.