Trivias
Trivia Description
Welcome to the Virosphere
In recent years, scientists have discovered that the world of virus diversity — what they sometimes call the virosphere — ...
The Fight Over Inoculation During the 1721 Boston Smallpox Epidemic
Although inoculations were themselves a risky practice and carried a not-insignificant health risk, this data demonstrates that inoculations were significantly ...
Spike in child hepatitis cases linked to common virus
Puzzled scientists are searching for the cause of a strange and alarming outbreak of severe hepatitis in young children.
The enigma of the 1889 Russian flu pandemic – a coronavirus?
The "Russian flu", which raged from 1889 to 1894, is considered as the first pandemic of the industrial era for ...
The relationship between GDP and life expectancy isn’t as simple as you might think
Accumulating evidence suggests that economic growth actually kills people.
What we can learn from the 1918 Flu Pandemic as the Omicron variant spreads
Historically, most pandemics end within 2 to 3 years as the virus mutates into a less virulent pathogen and the ...
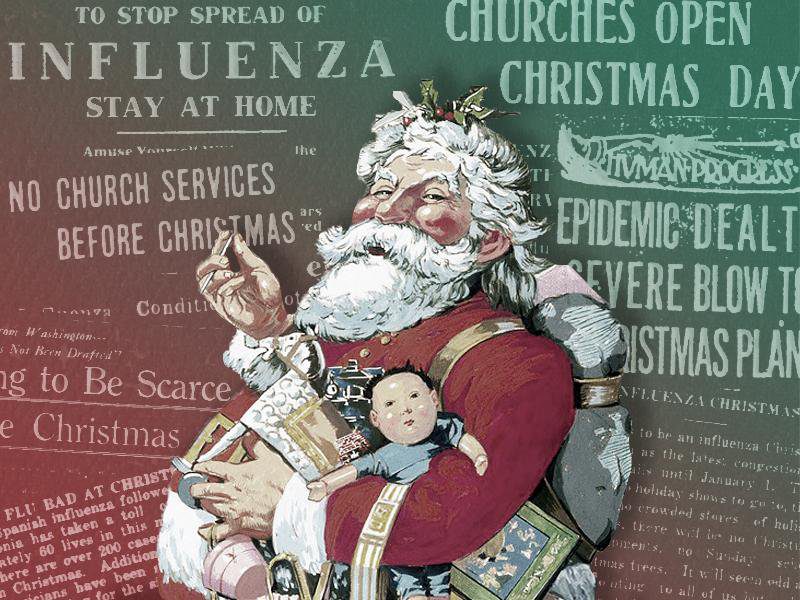
What pandemic Christmas of 1918 looked like
We take a trip back in time with Smithsonian Magazine to uncover the social and political issues affecting pandemic Christmas ...
This Thanksgiving, collect and share your family health history!
Happy Thanksgiving Day! It is time for our yearly message on the importance of family health history to your own ...
States have mandated vaccinations since long before COVID-19
Vaccination mandates in the U.S. date back to the 19th century, when many cities and states started requiring children to ...
How the Flu Pandemic Changed Halloween in 1918
Halloween is just not the same during any pandemic - and the changes we see now were also taking place ...
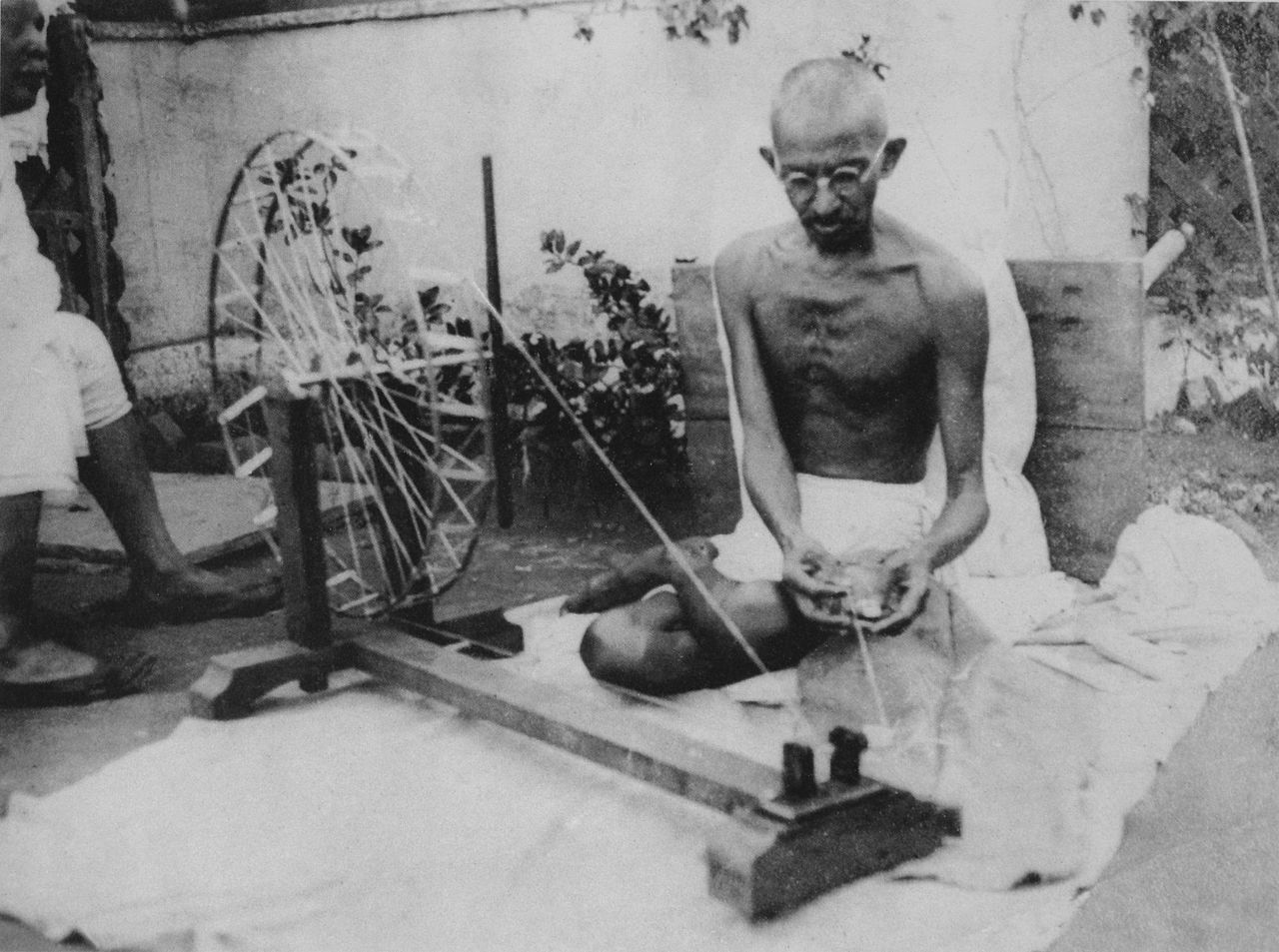
The Mahatma, an anti-vaxxer?
We chronicle the diaries of Mahatma Gandhi to learn about his personal views regarding vaccines.
Of Irrationality
Irrational beliefs differentially predict adherence to guidelines and pseudoscientific practices during the COVID-19 pandemic.